By the end of the year, 48 countries and territories of the Americas had reported more than half a million suspected cases of Zika, with 22 reporting some 2,500 cases of congenital syndrome associated with the virus.
 Washington, DC, December 29, 2016 (PAHO/WHO) – In 2016, Zika virus spread rapidly throughout the Americas after its initial appearance in Brazil in May 2015. The Pan American Health Organization (PAHO) responded quickly, deploying over 80 expert missions to help its Member States respond to the epidemic and launching a new regional strategy to prevent and control mosquito-borne viruses, which threaten an estimated 500 million at-risk people in the region.
Washington, DC, December 29, 2016 (PAHO/WHO) – In 2016, Zika virus spread rapidly throughout the Americas after its initial appearance in Brazil in May 2015. The Pan American Health Organization (PAHO) responded quickly, deploying over 80 expert missions to help its Member States respond to the epidemic and launching a new regional strategy to prevent and control mosquito-borne viruses, which threaten an estimated 500 million at-risk people in the region.
By the close of this year, 48 countries and territories in the Americas had reported more than 532,000 suspected cases of Zika, including 175,063 confirmed cases. In addition, 22 countries and territories reported 2,439 cases of congenital syndrome associated with Zika. Five countries had reported sexually transmitted Zika cases.
Zika, the first mosquito-borne flavivirus found to be also sexually transmissible and to cause birth defects, spread quickly. Before 2015, little was known about Zika apart from reports of earlier small outbreaks in Micronesia and French Polynesia. But the outbreak in Brazil’s northeast drew global notice and apprehension as graphic images of newborns with microcephaly, or smaller than normal heads, appeared widely.
PAHO Director Carissa F. Etienne recounted Zika’s sudden appearance in Brazil in May 2015 and its rapid spread throughout the Americas, noting, “No one could have imagined two years ago that our children would be affected by microcephaly as a result of this once-dormant villain.”
In a November 2016 keynote address to the American Society of Tropical Medicine and Hygiene, Etienne noted, “There is a still long way to go on Zika. The development of affordable new tools by the scientific community, including diagnostic tests and a vaccine against Zika, as well as innovation in vector control, is an urgent priority. Our health systems will need to be prepared to ensure such new tools are introduced and that their benefits reach everyone, not merely a few.”
In the Region of the Americas, “Zika was first confirmed while we were preparing for Ebola and responding to chikungunya,” Etienne said. “It was astute front-line healthcare workers who first realized that they were detecting something unusual. Indeed, our Zika experience proves once again that good clinical judgment and awareness of atypical events are crucial for the timely detection of emerging diseases. It also points to the importance of investing in the health workforce as the first line of defense against emerging disease threats,” she added.
Zika virus disease is caused by a virus that is mainly transmitted by infected female Aedes aegypti mosquitoes but also through sexual intercourse. People infected by Zika virus usually have mild symptoms that normally last for two to seven days and can include fever, skin rashes, conjunctivitis, muscle and joint pain, malaise or headaches. There is no specific treatment or vaccine currently available. The virus is now known to circulate in Africa, the Americas, Asia and the Pacific.
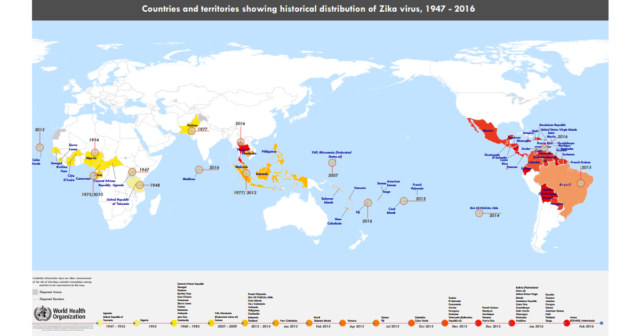
When clusters of babies with microcephaly and cases of Guillain-Barré syndrome were reported at the same time and place as Zika virus outbreaks, PAHO published a series of alerts starting in December 2015. Subsequently WHO declared a Public Health Emergency of International Concern (PHEIC) on February 1, 2016. Zika spread rapidly not only through the Americas but also to other regions. In all, 75 countries and territories now report evidence of mosquito-borne Zika local transmission since 2007, 13 countries have evidence of person-to-person transmission of Zika virus other than through mosquitoes, and 29 countries have reported microcephaly and other malformations.
Scientists and researchers also responded quickly, vastly increasing the world’s knowledge of this previously little-known virus. More than 1,500 research papers have now been published on Zika, confirming that the virus can infect mothers and unborn children and kill brain cells, causing a variety of birth defects. Researchers continue to find a widening range of effects in “congenital Zika syndrome,” including brain abnormalities, neural tube defects, eye abnormalities, hearing problems, irritability, seizures, feeding difficulties and others.
Experts now consider Zika to be a long-term public health challenge, following the declaration by WHO’s Emergency Committee on Zika that the epidemic’s emergency phase was over. Coordination and response activities by PAHO and WHO are being folded into longer-term efforts in detection, prevention, care and support. Further research is underway to strengthen preparedness and response in affected countries.
PAHO is providing technical support to its Member Countries in all aspects of Zika surveillance and control, with a special focus on clinical management, laboratory services and controlling the mosquito vectors of Zika virus, which also transmit dengue, chikungunya and urban yellow fever. Regional partners are involved in vector control research including pilot studies of new control methodologies such as mosquitoes infected by the Wolbachia bacteria. Community education and participation in eliminating mosquito vectors and breeding sites is a crucial tool in the long-term fight against Zika.
The Pan American Health Organization (PAHO) works with the countries of the Americas to improve the health and quality of life of their peoples. Founded in 1902, it serves as the WHO Regional Office for the Americas and is the specialized health agency of the inter-American system.
